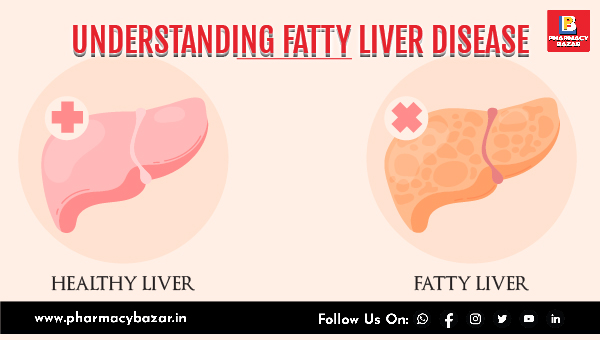
UNDERSTANDING FATTY LIVER DISEASE: CAUSES, SYMPTOMS, AND TREATMENT OPTIONS
Jun 02, 2023
The liver is a large, reddish-brown organ located in the upper right side of the abdomen in the human body. It is one of the most important organs in the body and plays a vital role in many of the body's functions.
The liver has a wide range of functions, including:
- Metabolism: The liver plays a crucial role in metabolizing nutrients from food, including carbohydrates, fats, and proteins. It converts glucose into glycogen and stores it for later use.
- Detoxification: The liver filters and removes harmful substances from the blood, including drugs, alcohol, and toxins.
- Production of bile: The liver produces bile, which helps in the digestion and absorption of fats in the small intestine.
- Storage: The liver stores important nutrients such as vitamins, minerals, and iron, and releases them into the bloodstream as needed.
- Regulation of blood sugar levels: The liver helps to maintain a stable level of glucose in the blood by producing and storing glucose and releasing it when needed.
- Production of clotting factors: The liver produces several clotting factors that are important for the formation of blood clots and stopping bleeding.
- Immune function: The liver plays a key role in the body's immune system by producing immune factors that help fight infection and disease.
Fatty liver is a most common liver disease also known as hepatic steatosis, is a condition characterized by the buildup of fat in the liver cells. This excess fat can cause inflammation and damage to the liver, leading to a range of health problems. Fatty liver can be caused by a variety of factors, including alcohol consumption, obesity, high cholesterol, diabetes, and certain medications. Fatty liver is often asymptomatic and can be detected through imaging tests, such as an ultrasound or CT scan, or through a blood test to measure liver function. In some cases, fatty liver can progress to more serious liver diseases, such as nonalcoholic steatohepatitis (NASH) or cirrhosis.
There are two main types of fatty liver:
- Non-alcoholic fatty liver disease (NAFLD): This is the most common type of fatty liver, and it is not caused by excessive alcohol consumption. It is often associated with obesity, insulin resistance, and metabolic syndrome.
- Alcoholic fatty liver disease (AFLD): This type of fatty liver is caused by excessive alcohol consumption. The amount of alcohol required to cause AFLD varies from person to person, but it generally takes years of heavy drinking to develop this condition.
The causes of fatty liver can vary, but some common causes include:
- Alcohol consumption: Heavy alcohol consumption is one of the most common causes of fatty liver disease.
- Obesity or overweight: People who are overweight or obese are at a higher risk of developing fatty liver disease.
- Type 2 diabetes: People with type 2 diabetes are more likely to develop fatty liver disease.
- High blood pressure: High blood pressure can lead to the development of fatty liver disease.
- High cholesterol or triglycerides: People with high levels of cholesterol or triglycerides in their blood are more likely to develop fatty liver disease.
- Rapid weight loss: Losing weight too quickly can cause the liver to release more fat than it can process, leading to fatty liver disease.
- Medications: Certain medications, such as corticosteroids and some chemotherapy drugs, can cause fatty liver disease.
- Genetics: Some people may be genetically predisposed to developing fatty liver disease.
It is important to note that in some cases, the cause of fatty liver disease may be unknown.
Fatty liver disease often causes no symptoms, especially in the early stages. However, as the disease progresses, the following symptoms may occur:
- Fatigue
- Weakness
- Weight loss or loss of appetite
- Abdominal pain and swelling
- Yellowing of the skin and eyes (jaundice)
- Swelling in the legs and ankles (edema)
- Mental confusion
- Spider-like blood vessels on the skin (spider angiomas)
- Redness of the palms of the hands
- Elevated liver enzymes on blood tests
It's important to note that not everyone with fatty liver disease will experience symptoms, and some people may not even know they have the disease until it's discovered during a routine medical exam or imaging test.
The treatment of fatty liver depends on the underlying cause and severity of the condition. Some common approaches to treating fatty liver include:
- Lifestyle changes: This involves adopting healthy lifestyle habits such as eating a healthy diet, losing weight, exercising regularly, avoiding alcohol and smoking, and controlling blood sugar levels.
- Medications: There are no specific medications to treat fatty liver, but your doctor may prescribe medications to treat underlying conditions such as diabetes, high cholesterol, or high blood pressure.
- Supplements: Some studies suggest that certain supplements, such as vitamin E, may help reduce liver inflammation in people with nonalcoholic fatty liver disease.
- Medical procedures: In rare cases, medical procedures such as liver biopsy or surgery may be recommended to diagnose or treat fatty liver.
It's important to note that treatment of fatty liver requires a comprehensive approach and regular monitoring by a healthcare provider. If you have been diagnosed with fatty liver, talk to your doctor about the best treatment options for you.
There are several drugs that can be used to treat fatty liver disease, but their effectiveness depends on the underlying cause of the disease. For example:
- Insulin-sensitizing agents: These drugs improve insulin sensitivity and are often used to treat people with nonalcoholic fatty liver disease (NAFLD) who have insulin resistance or type 2 diabetes. Examples include pioglitazone and rosiglitazone.
- Lipid-lowering agents: These drugs lower cholesterol and triglyceride levels in the blood and can help reduce the accumulation of fat in the liver. Examples include statins, fibrates, and omega-3 fatty acids.
- Antioxidants: These substances may help reduce inflammation and oxidative stress in the liver. Examples include vitamin E and betaine.
- Weight-loss drugs: In some cases, doctors may prescribe medications to help with weight loss, such as orlistat or liraglutide.
It's important to note that medication alone is not enough to treat fatty liver disease. Lifestyle changes, such as a healthy diet and regular exercise, are also crucial for managing the condition.
Fatty liver disease is becoming an increasingly common health problem worldwide, and its prevalence is estimated to be around 25% globally. Non-alcoholic fatty liver disease (NAFLD) is the most common form of fatty liver disease, and it is closely linked to obesity and metabolic syndrome.
The prevalence of NAFLD varies widely across different regions of the world, with the highest rates reported in Western countries such as the United States and Europe. In the United States, it is estimated that up to 30% of the adult population has NAFLD, and the prevalence is even higher in certain ethnic groups such as Hispanics.
The prevalence of NAFLD is also increasing rapidly in developing countries, particularly in Asia, where there is a high prevalence of obesity, diabetes, and other metabolic risk factors. In China, for example, the prevalence of NAFLD is estimated to be around 15-30%, while in India, the prevalence is around 9-32%.
The increasing prevalence of NAFLD is a major public health concern, as it can progress to more severe forms of liver disease such as non-alcoholic steatohepatitis (NASH), cirrhosis, and liver cancer. Effective prevention and management strategies are urgently needed to address this growing health problem.
DISCLAIMER: This article is the property of Pharmacy Bazar and is protected by copyright laws. The information provided in this article is for educational and informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article. The author and publisher of this article do not endorse any specific treatments, procedures, or products mentioned in this article.
Recent Post
Blood Cancer: Early Warning Signs and Diagnosis

Understanding Gallstones: Causes, Symptoms, and Treatment Options
Navigating Diabetes Medications: Benefits and Side Effects
Revolutionizing Cancer Treatment: How Unleashing T Cells' Energy Could Transform Immunotherapy

The Power of Lower Back Stretches: Benefits and Best Yoga Asanas for a Healthy Spine
8 Health Conditions That Could Be Due to Magnesium Deficiency

Unlocking Brain Health: How Lifestyle Choices Impact Cognitive Functions

When Speech Takes a Surprising Turn: Unraveling Foreign Accent Syndrome

The Optimal Time to Take Your Vitamin D Supplement: Insights and Best Practices

Beyond Diabetes: Unveiling the Hidden Health Risks of Insulin Resistance